1 In 3 Women Experience This Disorder But If We Said The Name In The Title You Wouldn’t Click In
It’s worth you yelling at us for that clickbait title because it’s just that important.
by The Candidly Team
If you’re a woman, your odds of experiencing this bitterly annoying condition are pretty astronomical.
We’re not gonna make you forage through 7 paragraphs to find out what it is, but before we let you scoot off, curiosity quenched, we will say this: our willingness to educate ourselves about it can hold the key to resolving it.
So here we are.
And here’s what it is: pelvic floor disorder.
Our pelvic floor is a muscle group that assists with some major functions, including:
Bladder and bowel control
Sexual function
Helping with circulation
Stabilizing the back, hips, and pelvis
Supporting the vagina, uterus, bladder, and bowels
As with any change to our body, experiencing symptoms around our pelvic floor is something we should get checked out by a doctor. That said, this is a very common condition and there are a ton of things we can do to intervene.
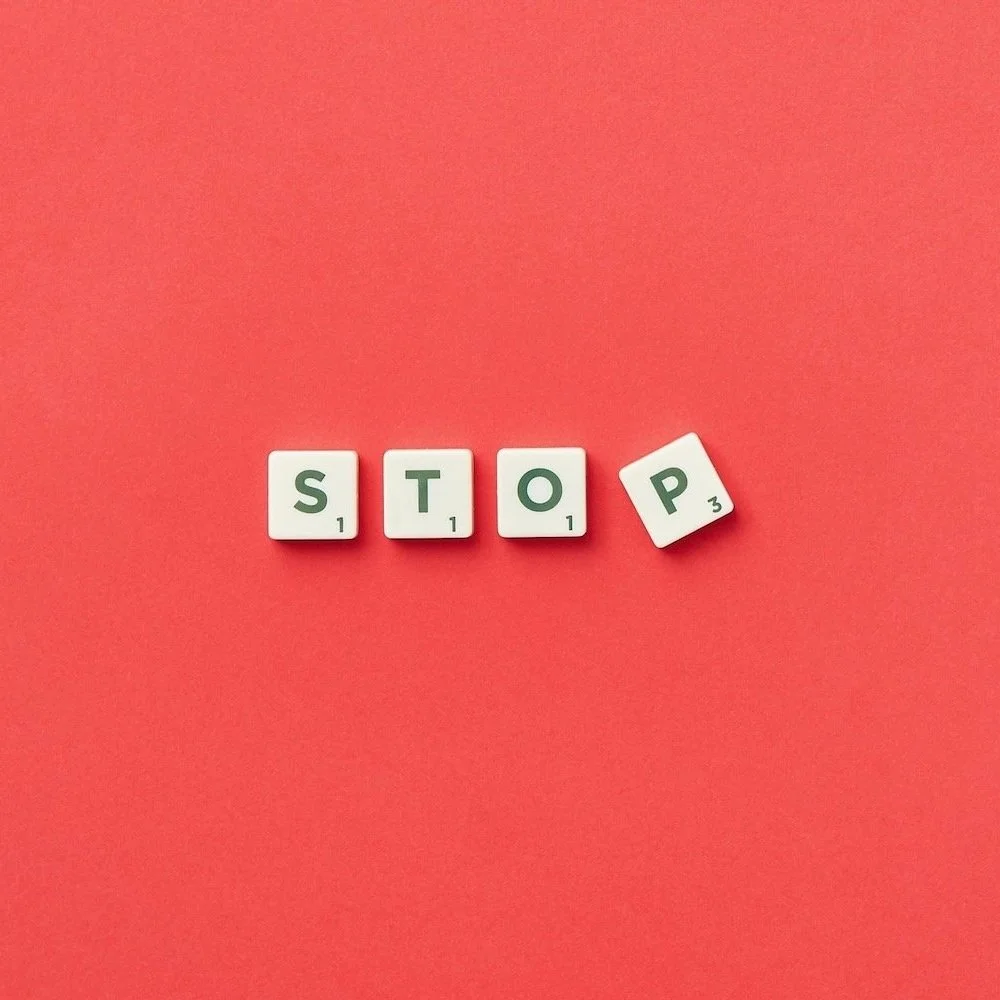
To outline exactly what those things are, we spoke to Dr. Celestine Compton of Origin, a physical therapy platform designed to target your pelvic floor. Her answers were wildly illuminating. And very, very hopeful!
1. To to start off, why should we care about our pelvic floor?
The reason we're talking about the pelvic floor right now is because, for a long time, we didn't. For most women in America, the expectation had been that, as we age, we would start to leak with coughing or sneezing, our vaginas may start to fall out, sex will not feel as good as it used to, and this is all just a part of getting old. And if you've ever had children, then you should expect these changes to happen a lot sooner.
As we've learned more about our bodies and seen more research, we now know that these "inevitable changes" are often actually just signs of neglect. If we care for our pelvic floor, just as we should care for the rest of our body, then many of these issues can be resolved or may never happen at all.
2. Given all the lovely hormonal shifts that take place in every stage of our lives, what changes can we expect to our pelvic floor after we hit 35? Feel free to not spare us the details.
Our pelvic floor is a group of muscles at the base of the pelvis. As we enter our 30s and 40s, the muscles in our body can begin to lose their mass, strength, and endurance partly because of:
Hormonal shifts: less estrogen leads to loss of muscle mass and degradation of the quality of our muscle fibers
Lifestyle changes: family, work and life demands coupled with fatigue and, likely, body aches and pains means our day to day life can get a lot more sedentary)
The normal aging process: In our mid-20s, our body is steadily building muscle mass, but by our 30s-50s, our body shifts from maintaining that mass to gradually losing muscle.
Obviously, our pelvic floor muscles are not immune to these changes, and when our pelvic floor begins to lose mass or strength, it can lead to changes in bladder, bowel, and sexual function.
At the same time, hormonal shifts related to perimenopause can further contribute to changes in each of these areas, leading to conditions such as vulvovaginal atrophy (VVA) and genitourinary syndrome of menopause (GSM).
Pelvic symptoms associated with VVA and GSM can include vaginal dryness, itching or burning, painful sex, frequent urination, painful urination or recurrent UTIs. If you’re experiencing any of these symptoms, reach out to your healthcare provider for support. While symptoms associated with hormonal shifts are not uncommon, they can be difficult to talk about; but speaking with your doctor is the first step to finding the treatment option that works best for you.
3. Are there any unexpected signs we should look for, aside from the usual suspects like peeing a little every time we sneeze?
If you notice any change to your bladder, bowel or sexual function, it is worth taking notice, because pelvic floor dysfunction can develop even before we experience the typical leaking with a sneeze.
For some people, pelvic floor dysfunction can begin to surface with rushing to the bathroom with urgency and panic after a long car ride or with leaking a little (urine or feces) while training for a marathon or with feeling the symptoms of a UTI even though cultures all come back negative.
If you are having more difficulty with achieving orgasm or if you have discomfort during sex but only in certain positions or if you feel the sensation of wearing a tampon when you go to lift something heavy, these may all be early signs of pelvic floor dysfunction.
4. Given that some of this is hormonal, are there real, proactive steps we can take to strengthen our pelvic floor? How would these activities rank from most to least effective in your opinion?
The first step to caring for and strengthening the pelvic floor is to understand the current condition of your own pelvic floor. Every body is different, so it is especially important to build understanding and confidence around knowing your pelvic floor, learn how to assess its ability and its limitations right now, consider what lifestyle factors may be contributing to your current condition, and what strategies and exercises will best help you to maintain or improve function as you age.
I encourage everyone to speak with a pelvic floor physical therapist in order to start this practice and learn: what is your awareness of your pelvic floor muscles and what is your level of control over them? What is their strength and how is their endurance? What is their range of motion and flexibility? And how do your pelvic floor muscles compare to "normal?"
Strengthening the pelvic floor can only happen once this first step is completed.
5. We all know about/ resent kegels. What are some other specific exercises we can try? Is it all about the pelvic floor or are there other muscle groups we should be honing in on?
If your biceps muscle (the one on your upper arm that you contract when people say "make a muscle") stops working well— maybe you were in a cast for 2 months, maybe you started a new job where you hold a leaf blower for hours at a time, maybe you’ve been carrying a 30lb baby on one elbow every day for the past 2 years— whatever the reason, if your bicep stops working, you do biceps specific stretches, massage, and bicep curls to restore your function. You can't restore function of your biceps without putting that muscle to work.
Kegels are the "bicep curls" of the pelvic floor. If your pelvic floor is not working, you can't avoid kegels but that likely isn't the whole story: I've never worked with anyone where the only thing they needed to get better was to "just do kegels."
Often, people with pelvic floor dysfunction will exhibit hip or core muscle dysfunction, as well. Or perhaps their urinary or digestive systems could use some help, or they may be carrying tension because of a high stress job or a personal trauma or loss.
Part of the goal of rehabilitating the pelvic floor is preventing dysfunction from returning again in the future, so addressing any surrounding issues is crucial for restoring and maintaining function.
With that in mind, keeping your glutes strong with bridges or squats and your core strong with bird dogs and deadbugs, which can be a great step towards improving pelvic stability
6. Any other lifestyle or just general tips we could be missing here?
The pelvic floor is just one part of the body. If those muscles start to dysfunction, it's worth considering what else may not be working in my body right now: Am I battling depression or anxiety? Am I still recovering from my knee replacement? Did I gain 20 lbs during the pandemic lockdown? Did I ever rebuild my leg strength after I broke my ankle playing soccer in high school? Am I entering menopause?
One of the best ways to care for your pelvic floor is to care for your whole body: reduce stress, eat well, sleep well, and exercise. But if you need additional support or guidance about how best to do that, reach out to a physical therapist who specializes in working with the pelvic floor— they are ready to help you figure out what is going on, what you can do about it, and what strategies can help prevent it from happening again.
This interview has been edited for length and clarity.
This article is for informational purposes only. It is not intended to be used in place of professional advice, medical treatment, or professional care in any way. This article is not intended to be and should not be a substitute for professional care, advice or treatment. Please consult with your physician or healthcare provider before changing any health regimen. This article is not intended to diagnose, treat, or prevent disease of any kind. Read our Terms & Conditions and Privacy Policy.